In the busy hallway of one of the health centers in the Amhara region of Ethiopia, I encountered Melat, a middle-aged woman whose tired eyes revealed the weight of her troubles. Despite living with diabetes for years, Melat’s understanding of self-management was rudimentary at best. Like many others in her neighborhood, she relied on a few prescription pills like metformin or insulin injections and irregular visits to the clinic to manage her condition. The everyday responsibilities of Melat’s hectic life continued to eclipse the idea of self-management, despite the seriousness of her condition. As we sat there, I couldn’t help but worry about Melat—a lady attempting to manage the complications of diabetes without the necessary tools she needs to succeed. Her experience provided a moving reminder of the urgent call to bridge the gap in diabetes self-management.
Diabetes has reached an epidemic status and is believed to be one of the most challenging
health problems in the 21st century. As with most non-communicable diseases, diabetes
now disproportionately affects people in low and middle-income countries, with 3 out of 4
diabetic patients residing in low-and middle-income countries (LMICs). The prevalence of diabetes in Ethiopia is 3.3%, representing one of the highest prevalence rates in sub-Saharan Africa.
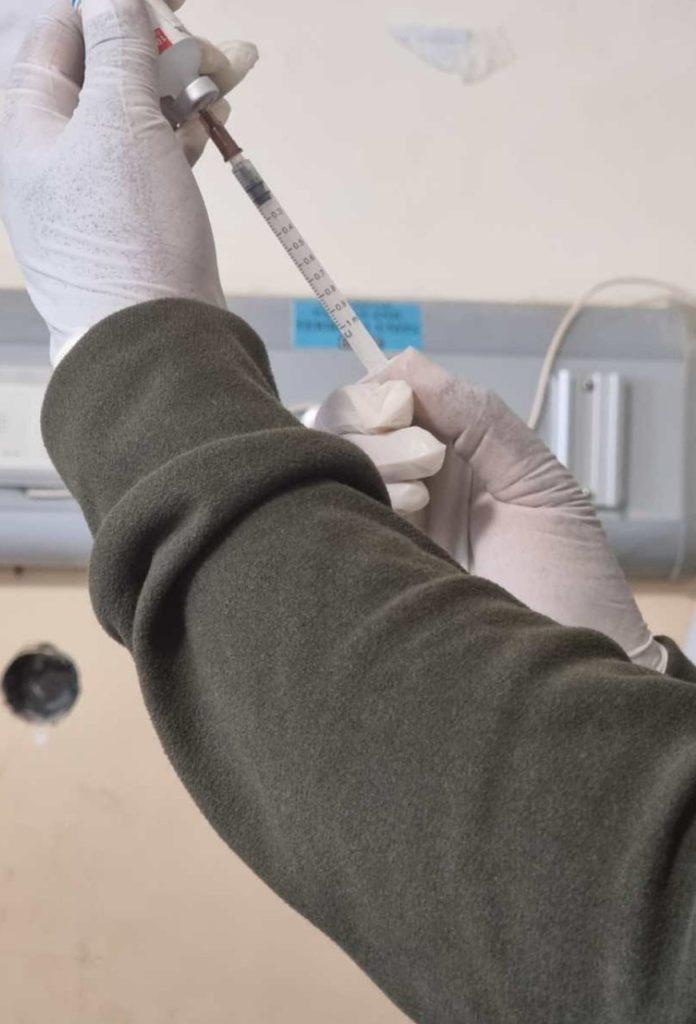
Self-management is a day-to-day activity that individuals with diabetes (ideally) engage in, which includes maintaining a balanced diet, regular blood glucose monitoring, and caring for one’s feet. Effective self-management not only complements medical treatment and follow-ups but also empowers individuals to take charge of their health, by promoting healthier lifestyles and reducing the burden of non-communicable diseases. As part of the 2030 agenda for sustainable development, member states have set an ambitious target to reduce premature mortality from NCDs – including diabetes – by one-third. According to WHO, increasing the effectiveness of self-management support may have a far greater impact on the health of the population than any other improvement in specific medical treatments.
However, recent studies show that self-management practices are poor in sub-Saharan Africa, including Ethiopia, highlighting a critical need for targeted interventions and educational programs to enhance diabetes self-management skills. This is particularly concerning considering that 80% to 90% of all care for people with chronic diseases is undertaken by individuals with diabetes themselves and their families.
Self-management support can be viewed in two ways: as a portfolio of techniques and tools
that help patients choose healthy behaviors; and a fundamental transformation of the patient-caregiver relationship into a collaborative partnership. However, several limitations hinder effective diabetes self-management in LMICs (and Ethiopia in particular), including a lack of organized diabetes care services, limited collaborative care practices, absence of multidisciplinary team care, inadequate training for healthcare providers, and limited availability of laboratory tests and medications. Despite improvements in availability and knowledge in diabetes care, the nuanced understanding of individual experiences and challenges when it comes to managing diabetes tends to be overlooked. Worse, many of them feel “lost in translation” in a maze of medical jargon and instructions. While there may be an improvement in medical knowledge and available interventions, the gap lies in translating this information into practical, actionable strategies and tools that resonate with individuals on a personal level. Some argue that investing in self-management requires significant resources. However, investing in self-management practices for diabetes can yield significant cost savings in the long run. By empowering individuals to manage their condition effectively, there is a reduced need for expensive medical interventions such as hospitalizations, emergency care visits, and long-term complications associated with uncontrolled diabetes.
Melat’s story highlights the often overlooked struggle of self-managing diabetes amidst a
(predominant) focus on medical treatment. It serves as a powerful reminder of the need to bridge the gap between medical expertise and the personal experiences of individuals facing this condition. A lot still needs to be done in this respect as despite the widespread prevalence of diabetes, particularly in countries like Ethiopia, effective self-management strategies remain elusive. Embracing a holistic approach to self-management support could empower people like Melat to confidently take control of their health. Among others, that would entail: simplifying education on diabetes management for better understanding and effective self-management; providing comprehensive training for healthcare providers in diabetes care in order to enable them to offer informed support and guidance; implementing community-based support programs; integrating technology for remote monitoring and consultations; developing culturally sensitive educational materials; establishing regular monitoring systems; and advocating for supportive policies. These would collectively enhance diabetes self-management in Ethiopia and similar settings, thereby improving health outcomes and quality of life for individuals with diabetes.
I believe such a holistic approach will help to ensure that individuals with diabetes feel no longer “lost in translation” in a maze of medical jargon and instructions. However, the responsibility shouldn’t fall on individuals with diabetes alone. The broader challenges of limited healthcare access, high medication costs, poor quality of services, and inadequate support systems all jeopardize self-management. By addressing these barriers with improved healthcare infrastructure, better quality of services, and supportive policies, we can empower individuals with diabetes to manage their condition more effectively and confidently.
Thank you so much …..You well articulated and explained what we were encountered such cases in daily bases as a physician.
Go a head my brother
Thanks Dr. Dereje. Great job!
A comprehensive outlook into one of the ever growing health challenges in our country Ethiopia, addressing many of the problems faced and providing solutions to better management of this complex disease. Well written