Chronic Respiratory Diseases (CRD) are a leading cause of death and disability worldwide. Just to give you an idea: in 2015, 3·2 million people died from one of the key CRDs, chronic obstructive pulmonary disease (COPD). Many of them occur in sub-Saharan African countries and other LMICs, and figures are on the rise. In addition, CRDs are also a significant cause of loss of productivity and high activity impairment, thus leading to decreased quality of life for many.
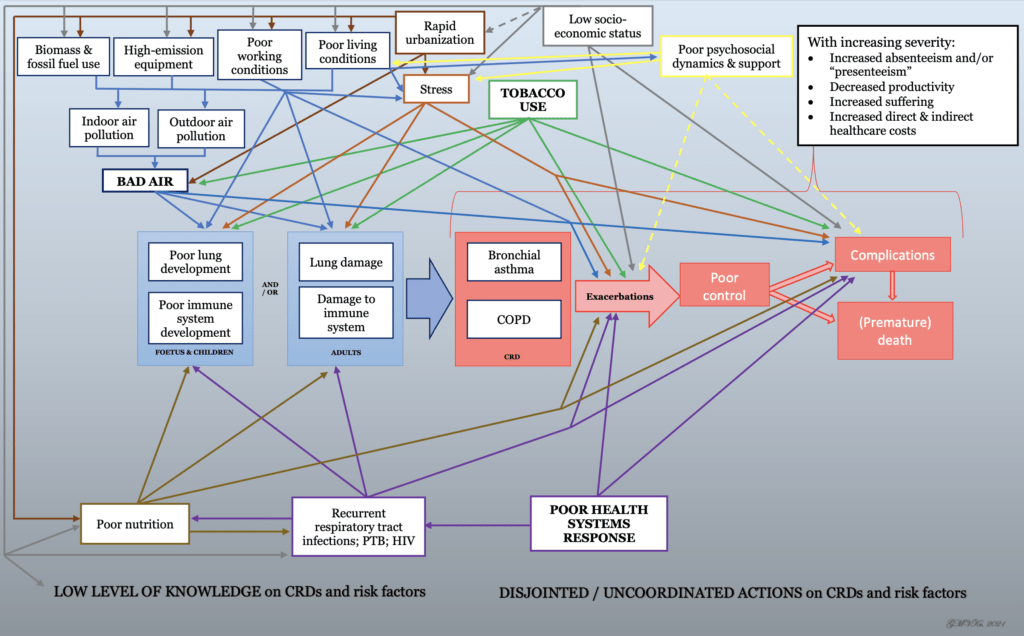
Sadly, akin to other NCDs, CRDs such as COPD and bronchial asthma are still thought to more commonly occur in high-income countries and largely due to poor lifestyle choices. However, CRD is a typical example of a condition caused by a multitude of social and structural determinants, and these societal and individual determinants are responsible for inequities in health.
Lung function is affected by lung size and abnormalities in structure. Unfavourable conditions influence lung (mal)development from foetal life; lung development continues after birth until early adulthood and both immature and mature lungs are susceptible to (further) lung damage throughout one’s lifetime.
Now, imagine this – the situation in a random LMIC:
All of these are common in LMICs. And all of these contribute towards sub-optimal respiratory health and well-being.
There are programs in place to address some of the above-mentioned determinants, such as tobacco (FCTC), HIV (90-90-90), PTB (global and national TB programs), etc., although implementation is currently deemed sub-optimal / not reaching targets. There are also attempts to strengthen health care provision for NCDs, but they focus more on diabetes, hypertension, and some cardiovascular diseases. Programs addressing other determinants beyond the health sector remain sporadic and “local”.
Multisectoral action needed
Air quality plays a significant role in the causation and worsening of CRDs; indoor, outdoor, household and industrial pollution – dirty exhausts from vehicles and factories, use of unclean fossil and biomass fuels, utilization of dirty cookstoves, poor waste management, use of incinerators, etc – are significant concerns that could be modified with appropriate action to control emission of noxious and harmful substances.
More rigorous implementation of tobacco control and translation of FCTC commitments into action is needed.
The same goes for adequate social protection, decent work and occupational health and safety.
Appropriate support and capacity strengthening of the health systems response to improve service delivery for CRDs and to address identified risks and promote health and well-being should be foreseen.
Engagement of patients and communities towards recognition of and propagating actions to address CRDs and associated determinants can be done, with special focus on women and children as they are more exposed to biomass smoke, targeted by Big Tobacco, etc.
It is important to note that acting on these challenges would help achieve a number of Sustainable Development Goals (SDGs 3, 5, 7, 8, 11, 12, 13, and 15).
In short, just as it takes a village to raise a child, addressing CRDs and determinants requires multisectoral action.
And the time to act was yesterday.